If you’re interested in having a baby, you already know that your menstrual cycle plays a big part in that whole “sperm meets egg” thing. But how do you know if what’s going on in your particular cycle is, well, ideal for baby-making? Here’s the real deal on your cycle—what’s normal, what’s not, and when it might make sense to get some medical help.
What a Typical Cycle Looks Like
A typical menstrual cycle is considered anywhere from 21 to 35 days, lasting three to seven days, with one to two days of heavier bleeding or cramping, says Dr. Alyse Kelly-Jones, a gynecologist in Charlotte, North Carolina. You will also see certain signs that you’re ovulating, like increased cervical fluid, a higher sex drive, or even a low-key ovarian pain that happens mid-cycle that can feel like a pinching, pulling, or aching.
Some of these changes might be subtle, so if you’re really curious, it’s a good idea to track your cycle to see what’s going on.
How Exactly Do I Track My Cycle?
If numbers and data aren’t your thing, you may need to think of cycle tracking more as a journey of self-discovery with a little science experimentation thrown in. The good news is that you have options! One way is to use one of those handy cycle apps, but just know you’ll need to do more than count the days between bleeds—you’ll also want to pay close attention to and track your body’s ovulation signs (or lack thereof). Again, this can include an increase in cervical mucus that’s clear, wet, and stretchy, breast tenderness, and a higher sex drive, per a 2017 study1 .
Another effective way to track ovulation is by regularly taking your body temperature when at rest—also called basal body temperature—which rises two to three days after you ovulate, according to the Mayo Clinic2 . To do this, you’ll need a specific thermometer that measures basal body temperature, which you will use to take your temperature every morning before you get out of bed. As you record these temperatures over a period of time, a pattern will emerge to help you identify when you’ll likely ovulate.
A third option is to use an ovulation prediction kit, which you can buy at your local pharmacy. This works similar to a pregnancy test in that they test your urine for a surge in hormones that occurs right before ovulation. Ovulation occurs about 36 hours after a positive result from one of these tests.
FYI, you only have to go in-depth on this stuff (and what we cover below) if you’re trying to conceive—or if you’re just really, really interested. It’s not mandatory for every cycling human!
What If I Find My Cycle Is Irregular?
Guess what? Not all menstrual cycles are the same, and that doesn’t necessarily mean your fertility is being affected. That said, there are some common reasons you may have an irregular period or cycle that you will want to check out with your healthcare provider. Here are a few to consider:
If your cycle is short
Although a normal menstrual cycle can be as short as 21 days, Dr. Kelly-Jones says she likes to see it closer to 23 days, particularly if you’re trying to get pregnant. If your cycle is shorter than this, it can indicate that you aren’t ovulating or that you aren’t making enough progesterone after you do ovulate, which is necessary to support a pregnancy.
Here’s why: If you’re TTC, you need progesterone to prepare the endometrium (lining of your uterus) for a fertilized egg. So if your progesterone level is low, that lining may not grow thick and strong, or it may come away too early—hence, the shorter cycle.
One other thing to consider is that shorter cycles, especially ones that shorten over time, are common as women age. A shorter cycle can be an indication of perimenopause.
If your cycle is long or missing altogether
If your cycle is longer than 35 days, it could be another indication that you’re not ovulating at all, says Dr. Kelly-Jones. This is called anovulation and it’s a problem because you need to release an egg in order to get pregnant. This often occurs due to hormonal imbalances from conditions like polycystic ovarian syndrome (PCOS). This is a common3 reproductive health issue that’s also a frequent cause of infertility. Don’t despair, though, as it can often be managed well with lifestyle changes, medication, or fertility treatments.
The same goes for if you don’t have any cycle at all. This is called amenorrhea, and can also occur due to certain medical conditions or low body weight. The caveat here is that if you’re on any sort of birth control or hormonal IUD, an absent cycle doesn't necessarily mean anything is wrong, but check in with your health care provider if you have concerns.
If you have very painful cycles
Pain is generally not normal, Dr. Kelly-Jones says. If you’re having unbearable cramps with your cycle, you should get checked out for endometriosis, an inflammatory condition in which tissue similar to the inside of the uterus grows outside the uterus. Other symptoms of endometriosis include painful sex or bowel movements, lower back and pelvic pain, and gastrointestinal issues, according to the Mayo Clinic4 .
And yes, endometriosis can affect your fertility (around 305 percent of women with infertility also have endometriosis). So, figuring out if you have this condition can be key to prepping your body for a future baby.
There are pain relievers and other drugs that can help make those painful periods a little more bearable, but Kelly-Jones recommends having an ultrasound and potentially seeing a specialist to see if further treatment like surgery is the right choice for you. Excision is a procedure that involves removing the endometriosis tissue to help manage the condition, and there is evidence that fertility improves after having this type of surgery, according to Brigham and Women’s Hospital6 .
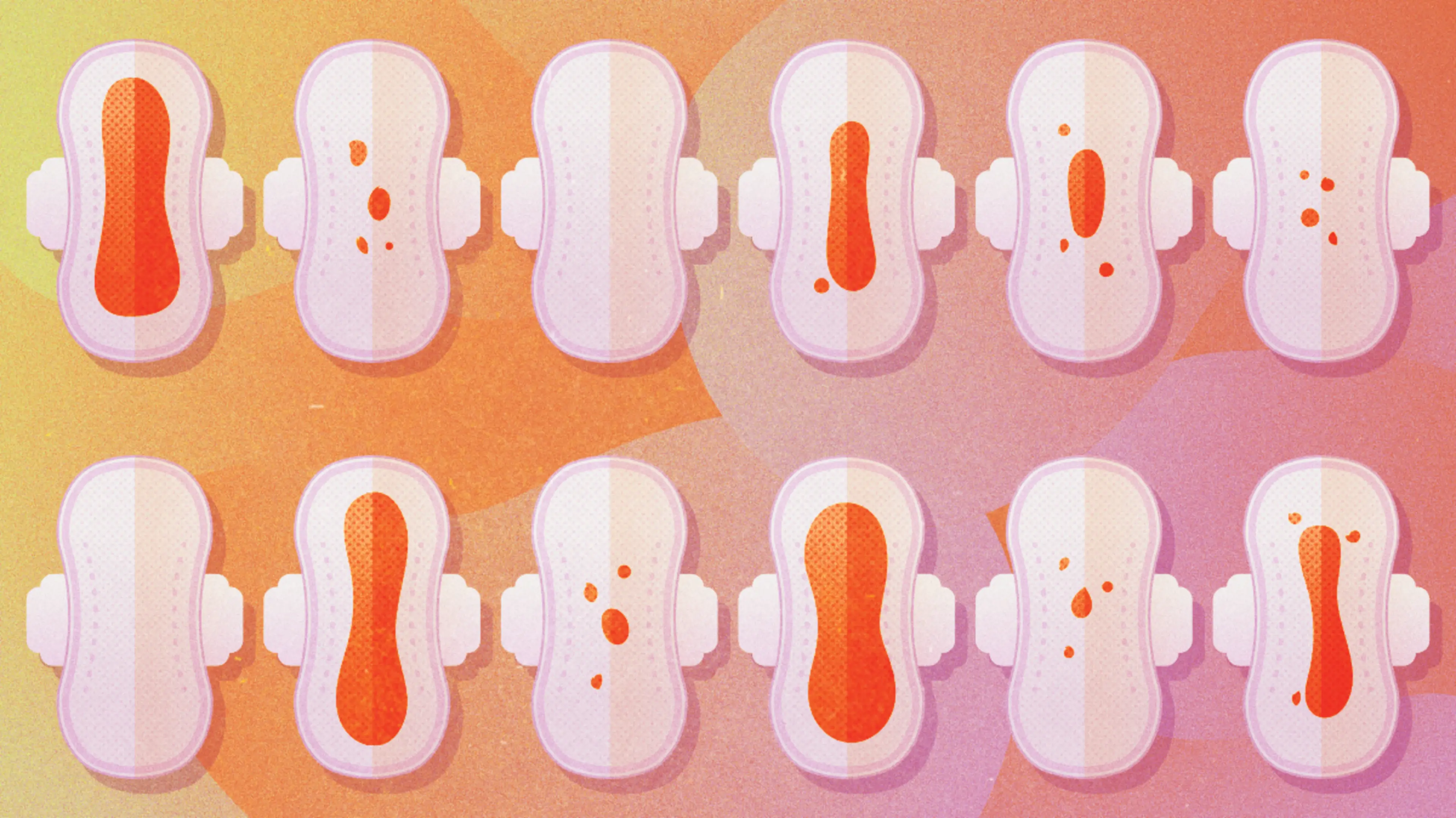
If you have heavy bleeding
Dr. Kelly-Jones explains that if she has a patient with heavy bleeding, her first thought is fibroids. (Though, causes of very heavy bleeding during a period can also be related to endometriosis or other uterine problems.) Fibroids are growths in the uterus made of muscle and tissue. They are fairly common during the reproductive years. They may affect people very differently, based on size of the fibroid, location of the fibroid, and other factors—some people may have pain, while others may not even know they have a fibroid.
Dr. Kelly Jones says fibroids may or may not affect your fertility, “depending on where the fibroids are located, how big they are, and if they are pushing on the lining of the uterus. Larger fibroids that are affecting the endometrium can affect not only fertility but the pregnancy itself once a woman gets pregnant.” Your doctor can talk you through treatment options if this is the cause of your heavy bleeding.
Spotting—a small amount of blood, aka not enough to use a pad, tampon, or cup—can be normal. If you spot towards the end of your period or as your period is beginning, that’s generally not an issue, especially if it’s for just a few days, says Dr. Kelly-Jones.
A bit of spotting in the middle of your cycle can be OK, too, says Dr. Kelly-Jones, and may even be something called “implantation bleeding,” if it happens after you’ve had unprotected sex during your fertile window. Read: You’re pregnant!
There are times when spotting may be a cause for concern, like if it lasts for a long time on either end of your period, Dr. Kelly-Jones explains. (Think spotting for five days before full bleeding begins or after it ends.) Sometimes, spotting can indicate something like a polyp or a fibroid. Other times, it may mean there’s something up with your hormones, including the possibility that you have low progesterone.
If you only spot occasionally, it’s probably nothing to worry about. But if you find your spotting is increasing or becoming your norm, that may indicate a change worth investigating.
If you have PMS or PMDD
In general, Dr. Kelly-Jones says that experiencing premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) won’t have a big effect on your actual physical fertility. Still, these conditions can sometimes be associated with low progesterone, so you may find it’s worth having your progesterone levels tested if you have either one.
There is also the mental health aspect of these two conditions, which Dr. Kelly-Jones says can “greatly affect your quality of life,” and, in turn, affect fertility. Think about it: If you’re stressed out about the emotional ups and downs you feel in the second half of your cycle or your daily functioning is affected by the depression and anxiety caused by PMDD, that’s probably not a great thing for baby-making. So, it may make a significant difference to get symptoms of these conditions under control before you start trying to conceive.
When To Get An Irregular Period Checked Out
There’s no need to worry if you experience a wonky cycle every once in a while. It’s totally normal to have a cycle that’s longer or shorter than your norm or a one-off bleed with killer cramps. After all, cycles are easily influenced by factors like stress, exercise, and illness. For Kelly-Jones, any change in your cycle that is consistent (her baseline is three cycles) is a reason to make an appointment with your provider, especially if you want to get pregnant in the future.
Be prepared to share about your concerns and come prepared with cycle tracking data, if you have it. While it’s true that normal menstrual cycles can look many different ways, trust yourself if something just doesn’t feel right. Remember—you’re always the expert on your own body.
Your provider may do a pelvic exam, order blood work, or give you an ultrasound to get to the bottom of your situation. Blood work can show quite a lot about what’s going on in your body, Kelly-Jones says. This goes beyond measuring your levels of estrogen and progesterone, she explains: “If a woman's thyroid is abnormal, for example, her cycle can go wonky. The same for prolactin levels. Both of those can negatively impact her fertility.”
Your menstrual cycle may check out to be A-OK, but chances are, you’ll be glad you made the appointment. After all, peace of mind can help a lot on the road to pregnancy.